Fighting for Research that Matters
In the pre-dawn hours, campus slumbers. But Ronan, a miniature schnauzer, is awake and ready to work. He hops out of the car, through the back door of Galvin Life Science Center, and pads down the hallway before donning his chemical booties and settling into his fireproof doggie bed in the Smith Lab. There, he appears to rest, but he’s on alert, waiting for signs that his owner, Nina Kikel-Coury, a biology graduate student, may have a seizure or faint. He’s always right, Kikel-Coury says, so when he nudges her, she puts down her beakers and sits on the floor, waiting for the moment to pass.
Kikel-Coury suffers from POTS, postural orthostatic tachycardia syndrome, an autonomic nervous system disorder that affects blood flow in between 1 million and 3 million Americans, typically women and young adults. Those numbers are growing as POTS and other forms of dysautonomia have been diagnosed as long-term impacts from COVID-19. The symptoms include fainting spells, seizures, respiratory issues and digestive trouble.
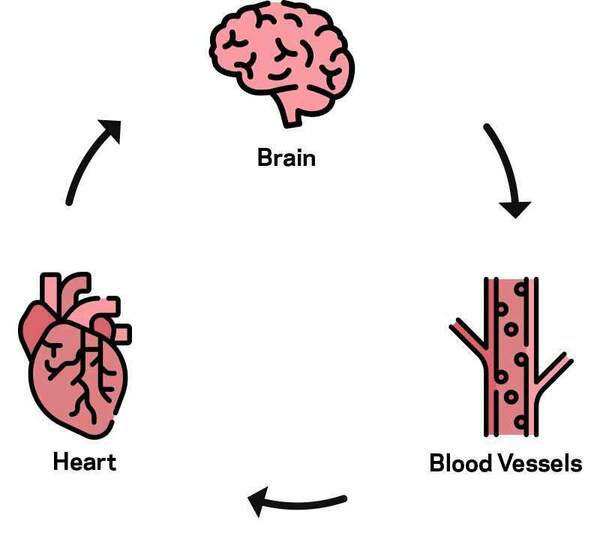 Heart rate and blood pressure work together to keep the blood flowing at a healthy pace, no matter what position the body is in. People with POTS can't coordinate the balancing act of blood vessel squeeze and heart rate response. This means the blood pressure can't be kept steady and stable.
Heart rate and blood pressure work together to keep the blood flowing at a healthy pace, no matter what position the body is in. People with POTS can't coordinate the balancing act of blood vessel squeeze and heart rate response. This means the blood pressure can't be kept steady and stable.To understand POTS, picture a thermostat, explains Kikel-Coury. You set a temperature, and then the machinery works to maintain that temperature, even as environmental conditions work against it. In people, the autonomic nervous system functions as that thermostat.
“In my particular case my thermostat is broken, so it doesn’t read the temperature. And if it’s cold, it’s actually going to think it’s hot; if it’s hot it’s going to think it’s cold. So that ultimately makes it so that none of my bodily functions work correctly.”
This rendered her high-risk during the COVID-19 pandemic, making collaborative research, a hallmark of Notre Dame’s graduate school, challenging. But her mentor, Cody Smith, the Elizabeth and Michael Gallagher Associate Professor of Biological Sciences and a member of the Center for Stem Cells and Regenerative Medicine, was undeterred. He established “Nina hours” in his lab when she could safely do experiments alone and then return home before others started their day. If she needed assistance during business hours, lab mates happily stepped in and sent her results via email or FaceTime.
“I have a mentor who completely understands my situation and really thinks outside the box so that I can reach my goals, goals that I’ve had since I was a kid,” she says. “Part of the reason I joined Notre Dame is because it felt like such a tight-knit community, and in particular with my lab, we are a family.”
She adds, “Lauren [Green] in particular in my lab has been an absolute lifesaver. She has helped cross my zebrafish for experiments. She has helped image my gels when I cannot. And throughout all of that she’s never made me feel like I’m a burden. She’s advocating for me, as a friend and as a scientist.”
 Nina safely does experiments alone in the Smith Lab during “Nina hours.”
Nina safely does experiments alone in the Smith Lab during “Nina hours.”
 Lauren Green, one of Nina's lab mates, video chats with Nina.
Lauren Green, one of Nina's lab mates, video chats with Nina.
That collaboration within labs, groups and colleagues is exactly what the Graduate School champions, says Dean Laura Carlson.
“The fact that Nina’s lab mates and Cody set an excellent example of servant leadership here, and the fact that they have stepped in and tried not just accommodating her, but actively are helping her reach her goals, is completely consistent with a community focus.
“It’s part of our ethos at Notre Dame,” she says.
“There is a recognition that when the community is strong, individuals within that community become stronger—it’s a dynamic system, with individuals giving to and receiving from the community. It’s about the community more than being about yourself.”
“There is a recognition that when the community is strong, individuals within that community become stronger.”
Carlson explains that the school cultivates a servant leader model that is built upon the idea that by working together, even greater good can be achieved.
“In a servant leader model, you bring your team along to a greater good. It’s not about you, the leader—it’s about your team and it’s about the goal and the good that you’re trying to bring to the world,” she says.
That good, in the case of Kikel-Coury, has been a profound discovery: a previously undetected cell in the heart that coincidentally may contribute to dysautonomia like POTS.
“What I found is that this new glial cell called cardiac nexus glia actually functions with the autonomic nervous system to regulate heart rate and heart rhythm,” she explains. “What we found is that if these cells are not present in the heart, it’s going to lead to an increase in heart rate as well as rhythm defects. And ultimately we found that this cell also functions with the autonomic nervous system to achieve this cardiac homeostasis.”
Kikel-Coury explains that a majority of glial cells, a focus of Smith’s lab, were previously thought to reside in the central nervous system and were largely explored in other organs. The discovery of a glial cell in the heart could lead to unexpected progress in cardiac research.
“Identifying cardiac nexus glia could have a huge impact, not only with the neuroscience field but also the cardiovascular field,” she says. “Currently no one knows why dysautonomia occurs in a lot of people. And so personally it’s really exciting to know that maybe we’re just one step closer to figuring out the cause of dysautonomia, and in particular, long term down the road maybe even POTS.”

Research that matters
Research like Kikel-Coury’s is precisely the kind of work the graduate school encourages, says Carlson. She explains that the Graduate School has truly embraced Notre Dame’s mission to be a force for good in the world, and it expects students to use that purpose to guide their research. This is made tangible to students through innovative training programs like the nationally recognized Leadership Advancing Socially Engaged Research program that emphasizes social responsibility as an essential element of their doctoral training.
“We attract students who think about impact as an important aspect of their research and the way in which they decide what questions to ask,” Carlson says. But she makes an important distinction: The research does not need to be applied in nature. Basic research, or research that is four, five, 10 steps away from application, is crucially important. The expectation is that students envision an important end goal for their work, even if they are not the one to execute it.
That’s the case for Kikel-Coury. The discovery of the cell is basic biology research, but she hopes that by publishing and making her work public, someone else can build upon her discovery to help others. She plans to pursue a job in science communication after graduation.
Carlson also underscores that the University takes a firm view of students’ intrinsic value.
“One of the things that makes training unique at Notre Dame is our holistic training model. We want you to be healthy and well, both in terms of your academic pursuits and in terms of your spiritual, emotional, financial, physical, social, emotional health,” she says. “You matter because you are a person, not just because you’re a researcher.”
