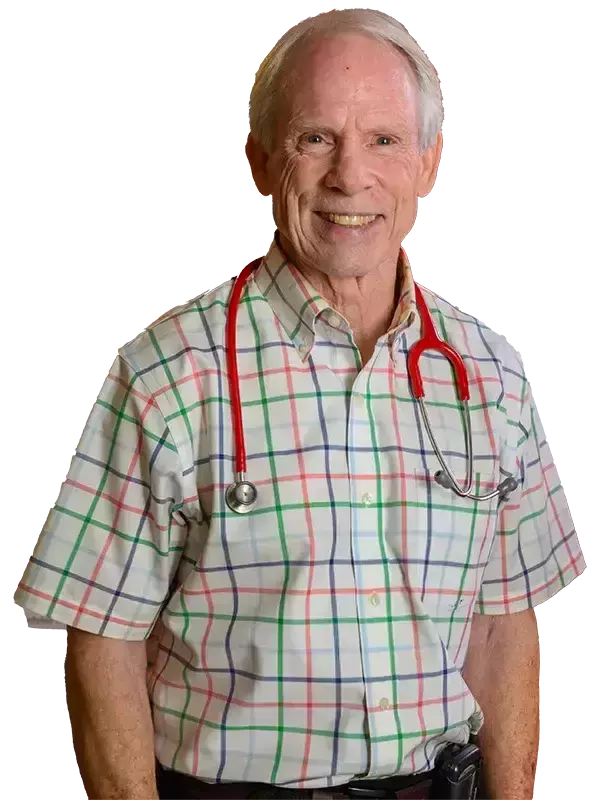
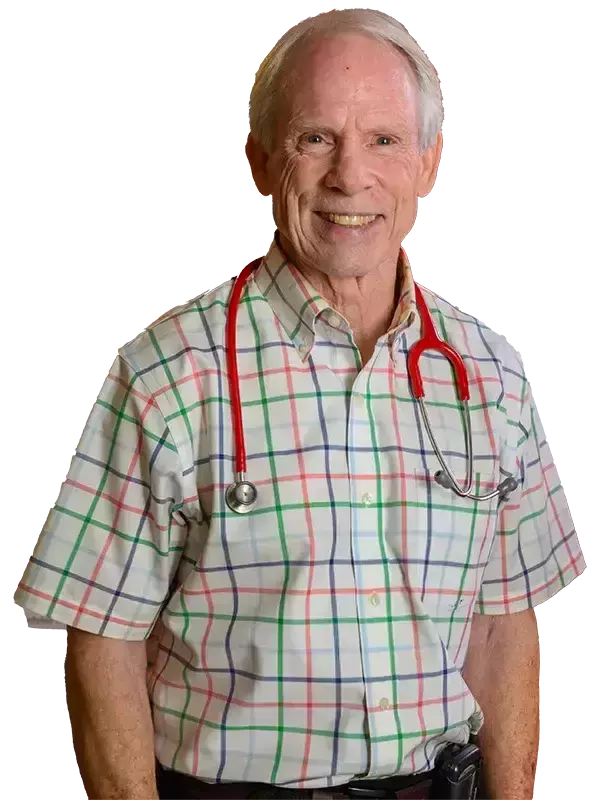
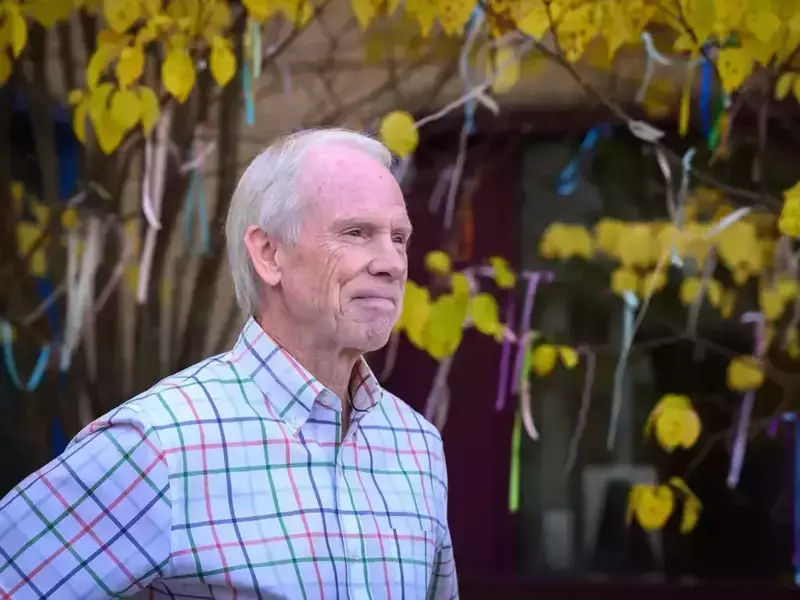
During his early years as a neonatologist in the 1970s, Dr. Bob White recalls bassinets lined up along the walls of the newborn intensive care unit while nurses looked on like hawks.
Babies were prodded regularly for tests and treatments. Doctors rushed in to the sound of alarms, scaring not just the family whose baby was in distress, but any family looking on. Though normal at the time, even then White knew things needed to change.
“It was kind of a culture shock to walk into that. Even as a medical person, I was immediately overwhelmed by sights and the noise and the bright lights. So it didn’t take me long to figure out this wasn’t the ideal environment for babies to be healing,” he remembered.
“The other piece that was starkly obvious was the absence of families. Back then, we had these preconceived notions that families would bring in germs that would be dangerous to babies—bacteria of various sorts—so we shouldn’t let them touch them.”
Breast milk, too, was taboo in the NICU, he recalled.
“We’ve gone 180 degrees on all of those!” he laughed.
Durante sus primeros años como neonatólogo en la década de 1970, el Dr. Bob White recuerda cunas alineadas a lo largo de las paredes de la unidad de cuidados intensivos para recién nacidos mientras las enfermeras observaban como halcones.
A los bebés se les pinchaba periódicamente para hacerles pruebas y tratamientos. Los médicos acudían apresuradamente ante el sonido de las alarmas, asustando no sólo a la familia cuyo bebé estaba en peligro, sino a todos los familiares que estaban presentes. Aunque en ese momento era normal, incluso entonces White sabía que las cosas tenían que cambiar.
“Fue una especie de choque cultural entrar allí. Incluso como persona del área médica, inmediatamente me sentí abrumado por la apariencia, el ruido y las luces brillantes. Así que no me llevó mucho tiempo darme cuenta de que ese no era el entorno ideal para que los bebés se curaran”, recordó.
“El otro elemento que resultó absolutamente evidente fue la ausencia de las familias. En aquel entonces, teníamos ideas preconcebidas de que las familias traerían gérmenes que serían peligrosos para los bebés (bacterias de varios tipos), por lo que no debíamos dejar que los tocaran”.
La leche materna también era un tabú en la UCIN, recordó.
“¡Hemos dado un giro de 180 grados en todos estos aspectos!” dijo riendo.

But change didn’t happen overnight.
White received his undergraduate degree from Notre Dame in 1971. After medical school at Johns Hopkins and a stint in Niles, Michigan, White returned to South Bend as a neonatologist hired to create a NICU at what is now Beacon Children’s Hospital. It occurred to him that some of the concerning concepts he had observed in NICUs could be studied and quantified, so he reached out to Notre Dame psychology professor Tom Whitman to begin a partnership with the Department of Psychology. White became adjunct faculty and has remained a beloved instructor for 34 years.
Pero el cambio no se produjo de la noche a la mañana.
White recibió su título universitario de Notre Dame en 1971. Después de asistir a la facultad de medicina en Johns Hopkins y de una rotación en Niles, Michigan, White regresó a South Bend como neonatólogo contratado para crear una UCIN en lo que ahora es el Beacon Children’s Hospital. Se le ocurrió que algunos de los conceptos preocupantes que había observado en las UCIN podrían estudiarse y cuantificarse, por lo que acudió al profesor de psicología de Notre Dame, Tom Whitman, para iniciar una alianza con el Departamento de Psicología. White se convirtió en profesor adjunto y ha seguido siendo un instructor muy querido durante 34 años.
Notre Dame Researchers
The many leaps in better NICU care are thanks in part to a number of Notre Dame researchers. They include:

Kathleen Kolberg
Associate dean, College of Science
Kolberg has long assisted with the NICU standards as an administrator, and her research on environmental stressors for prenatal and early postnatal development has helped shape many of the recommendations.

Tom Whitman
Professor emeritus, Department of Psychology
Whitman facilitated the collaborative research efforts between Notre Dame and Beacon and helped create the Psychology and Medicine course.

Jim McKenna
Faculty emeritus, Department of Anthropology
McKenna, a world-renowned expert on infant sleep, founded the Mother-Baby Behavioral Sleep Laboratory to study infant sleep, mother-baby co-sleeping, breastfeeding, and risk factors for SIDS. His work was instrumental in proving the importance of private family rooms in NICUs to facilitate bonding.

Lee Gettler
Professor and chair, Department of Anthropology
Gettler is the director of the Hormones, Health, and Human Behavior Lab where he focuses on men’s hormone physiology responses to life transitions, including fatherhood. He has also continued McKenna’s research on co-sleeping, especially as it pertains to the role of fathers.

Dominic Vachon
The John G. Sheedy, M.D., Director of Notre Dame’s Ruth M. Hillebrand Center for Compassionate Care in Medicine
Vachon is a practicing psychologist whose specialty is in the relationship between empathy and burnout in medical providers and helping professions. He has also advised Beacon’s NICU team in a compassionate care approach.
Los investigadores de Notre Dame
Los numerosos avances en la mejora de la atención en la UCIN se deben en parte a varios investigadores de Notre Dame. Entre ellos se incluyen:

Kathleen Kolberg
Decana asociada, Facultad de Ciencias
Kolberg ha colaborado durante mucho tiempo con los estándares de la UCIN como administradora, y su investigación sobre los factores ambientales estresantes para el desarrollo prenatal y posnatal temprano ha ayudado a dar forma a muchas de las recomendaciones.

Tom Whitman
Profesor emérito del Departamento de Psicología
Whitman facilitó los esfuerzos de investigación colaborativa entre Notre Dame y Beacon y ayudó a crear el curso de Psicología y Medicina.

Jim McKenna
Profesor emérito del Departamento de Antropología
McKenna, un experto de renombre mundial en el sueño infanti,l fundó el Laboratorio de comportamiento del sueño madre-bebé para estudiar el sueño infantil, el colecho madre-bebé, la lactancia materna y los factores de riesgo del SMSL. Su trabajo fue fundamental para demostrar la importancia de las habitaciones familiares privadas en las UCIN para facilitar el vínculo.

Lee Gettler
Profesor y director del Departamento de Antropología
Gettler es el director del Laboratorio de Hormonas, Salud y Comportamiento Humano, donde se centra en las respuestas de la fisiología hormonal de los hombres a las transiciones de la vida, incluida la paternidad. También ha continuado la investigación de McKenna sobre el colecho, especialmente en lo que respecta al papel de los padres.

Dominic Vachon
Dr. John G. Sheedy, director del Centro Ruth M. Hillebrand para la Atención Compasiva en Medicina de Notre Dame
Vachón es un psicólogo en ejercicio cuya especialidad es la relación entre la empatía y el agotamiento en el personal médico y las profesiones de apoyo. También ha asesorado al equipo de la UCIN de Beacon en un enfoque de atención compasiva.
One of the first things they studied was the lighting. Now the director of the regional newborn program at Beacon, White recalled NICUs had few, if any, windows and little natural light. Fluorescent lights remained on 24/7. What’s more, hospital code prevented putting cribs too near the windows for fear of the fragile babies catching cold and losing energy.
“The first thing we did was to determine whether or not babies would do better if you gave them a daylight cycle. So our room had big skylights which gave them natural lighting during the day and then turned the lights down at night. Then we conducted a randomized, controlled trial which showed that babies did do better if they had a circadian rhythm,” he said. “What we didn’t study, but was also equally obvious, was that all the staff and all the families loved it.”
White explained that the trial’s results showed that babies given cycled light saw increased weight gain, spent fewer days on a ventilator, and started oral feedings sooner. They were also discharged several days earlier than babies kept in a continuous environment of bright lighting.
Based on these results, the team set out to change the codes to encourage natural light, or at least cycled light, in NICUs. To do so, they put together a committee of experts including architects, hospital administrators, and researchers such as Kathleen Kolberg, now an associate dean in the College of Science, and published the data on their research.
Una de las primeras cosas que estudiaron fue la iluminación. White, ahora director del programa regional para recién nacidos en Beacon, recordó que las UCIN tenían pocas ventanas (si es que tenían alguna) y poca luz natural. Las luces fluorescentes permanecían encendidas las 24 horas del día, los 7 días de la semana. Además, el código hospitalario impedía colocar las cunas demasiado cerca de las ventanas por temor a que los frágiles bebés se resfriaran y perdieran energía.
“Lo primero que hicimos fue determinar si los bebés crecerían mejor si se les daba un ciclo de luz diurna. Entonces nuestra habitación tenía grandes tragaluces que proporcionaban iluminación natural durante el día y luego apagaban las luces por la noche. Luego realizamos un ensayo controlado aleatorio que demostró que a los bebés les iba mejor si tenían un ritmo circadiano”, dijo. “Lo que no estudiamos, pero que también fue igualmente evidente, fue que a todo el personal y a todas las familias les encantó”.
White explicó que los resultados del ensayo mostraron que los bebés que recibieron ciclos de luz tuvieron mejor aumento de peso, pasaron menos días conectados a un respirador y comenzaron a alimentarse por vía oral más pronto. También fueron dados de alta varios días antes que los bebés mantenidos en un entorno continuo de iluminación brillante.
Basándose en estos resultados, el equipo se propuso cambiar los códigos para fomentar la luz natural, o al menos la luz ciclada, en las UCIN. Para ello, crearon un comité de expertos que incluía arquitectos, administradores de hospitales e investigadores como Kathleen Kolberg, ahora decana asociada de la Facultad de Ciencias, y publicaron los datos de su investigación.
The NICU unit at Beacon Children’s Hospital features amenities that promote close physical contact between premature babies and their parents. Missing from this photo are the windows to the outside that provide natural light that helps babies maintain circadian rhythms, and the pullout sofa sleeper that provides space for two people.
That once-small committee grew and grew. Now it’s a large professional group including neonatologists, parents, nurses, doctors, architects, hospital planners, and basic scientists with specialties in lighting, sound, sociology, and more. Institutions including Cornell, Baylor, Ohio State, and University of Colorado contribute, as do international groups. Together, they systematically review the best practices of how to build and run NICUs.
Since 1992, this multidisciplinary team has translated those requests into actionable items for NICU design. The result is the Recommended Standards for Newborn Intensive Care Unit Design, which recently released its 10th edition. These standards are disseminated internationally and influence the design of NICUs worldwide.
“We were not just saying this would be a nice thing to do. There was evidence that this gives better outcomes.”
Dr. Bob White
White and Kolberg also help lead an annual conference, now called the Gravens Conference, which is in its 38th year. The conference welcomes medical professionals, researchers, hospital administrators, families, architects, and others to an annual conference to discuss best practices in NICU settings.
Together, the groups have advocated for private rooms for NICU families, as well as couplet care rooms where mothers can receive their postpartum care alongside their newborn. In 2017, Beacon became the first US hospital to install those rooms. The group has shown the efficacy of breast milk and the importance of parent bonding in a baby’s earliest days. Their recommendations cover everything from appropriate signage to acoustics, furnishings to handwashing. No detail seems too small.
Jay and Elizabeth Tipton have experienced the improved NICU firsthand. Their twin boys, Alexander and Benjamin, spent nine days in Beacon’s NICU after being born at 35 weeks and three days. There, the boys worked on stabilizing their temperature and blood sugar before they could go home to join their older siblings.
As they were ushered into a private suite, Jay, a nurse in the hospital’s surgery department, was wowed by how intentional the room design was. He recalled being impressed by the silent alarms that would ping a nurse’s phone rather than setting off a startling alarm in the room, and by how medical equipment was strategically masqueraded to reduce stress levels. Even details like large windows seemed novel, but purposeful, in a hospital setting.
Ese comité, que alguna vez fue pequeño, creció y creció. Ahora es un gran grupo profesional que incluye neonatólogos, padres, enfermeras, médicos, arquitectos, planificadores de hospitales y científicos básicos con especialidades en iluminación, sonido, sociología, entre otras. Contribuyen instituciones como Cornell, Baylor, Ohio State y la Universidad de Colorado, así como grupos internacionales. Juntos, revisan sistemáticamente las mejores prácticas sobre cómo construir y gestionar las UCIN.
Desde 1992, este equipo multidisciplinario ha traducido esas solicitudes en elementos aprovechables para el diseño de las UCIN. El resultado son las Normas recomendadas para el diseño de unidades de cuidados intensivos neonatales, que recientemente lanzó su décima edición. Estas normas se difunden internacionalmente e influyen en el diseño de las UCIN en todo el mundo.
“No sólo dijimos que sería bueno hacer esto. “Hay evidencia de que esto da mejores resultados”.
Dr. Bob White
White y Kolberg también ayudan a dirigir una conferencia anual, ahora llamada Conferencia de Gravens, que se encuentra en su 38º año. La conferencia recibe a profesionales médicos, investigadores, administradores de hospitales, familias, arquitectos y otros interesados a una conferencia anual para discutir las mejores prácticas en entornos de UCIN.
Juntos, los grupos han abogado por habitaciones privadas para las familias de la UCIN, así como salas de cuidados conjuntos donde las madres pueden recibir su atención posparto junto con su recién nacido. En 2017, Beacon se convirtió en el primer hospital de EE. UU. en disponer de esas habitaciones. El grupo ha demostrado la eficacia de la leche materna y la importancia del vínculo con los padres en los primeros días de vida del bebé. Sus recomendaciones abarcan todo, desde la señalización adecuada hasta la acústica, el mobiliario y el lavado de manos. Ningún detalle parece demasiado pequeño.
Jay y Elizabeth Tipton experimentaron de primera mano la mejora de la UCIN. Sus hijos gemelos, Alexander y Benjamin, pasaron nueve días en la UCIN de Beacon después de nacer a las 35 semanas y tres días. Allí, los niños se enfocaron en estabilizar su temperatura y nivel de azúcar en sangre antes de poder regresar a casa para reunirse con sus hermanos mayores.
Cuando los condujeron a una suite privada, Jay, un enfermero del departamento de cirugía del hospital, quedó sorprendido por el diseño tan especializado de la habitación. Recordó que le impresionaron las alarmas silenciosas que hacían sonar un pequeño timbre en el teléfono de la enfermera en lugar de activar una alarma ruidosa en la habitación, y cómo el equipo médico estaba estratégicamente oculto para reducir los niveles de estrés. Incluso detalles como las ventanas grandes parecían novedosos, pero útiles, en un entorno hospitalario.
“[There were] great big windows allowing lots of natural sunlight to come in during the day and make it feel less like you’re in a hospital. I can’t tell you how much of a difference that makes,” Tipton said. He recalled watching a Midwestern storm roll in and being comforted by watching the outside world moving. “It reminds you that this tiny room isn’t all there is.”
Inside that tiny room can be stressful. Tipton said the boys needed nasogastric tubes that run from the nose to the stomach to supplement what they could take from a bottle. At first, the nurses handled those feedings, but in time, he grew to feel confident he could take over.
“The nurses really encouraged us to be involved in the care of our sons as much as we wanted to be. Whether it was feeding them or changing them or bathing them, they didn’t allow us to be paralyzed or sidelined by our uncertainty or any fear. They really encouraged us to take hold of parenting and giving care to our boys.
“The couplet care room concept provides an opportunity for you to start practicing what care is going to be like at home, even in the hospital setting with the support of the nursing staff. So it’s almost like having training wheels for when you bring your baby home. It’s an opportunity for you to practice and to learn and to be able to make sure that you are prepared for success and your baby’s prepared for success when you get home,” he said.
Thankfully, the Tipton boys remained in the NICU for only nine days before they were discharged, but Jay recalled that other families on the floor had been there much longer, turning their private rooms into an extension of their home. That was welcome, if not encouraged, he said, and made the experience more comfortable.
But what sticks with him now was the staff, especially Dr. White.
“The thing that sticks in my memory that I will never ever forget: He would come every single morning during rounds and he would be in the room as long as we needed to talk to us, let us know what our goals were for the day, answer our questions. And when he would leave, he would always sort of turn back and look as he was walking away and say, ‘It’s the best job in the world.’ And he really meant it. You could tell that was not just something that he was saying,” Tipton said. “You can’t quantify what that means as a patient to have a physician who is not only that invested, but one who has that much joy in what they do.”
“Había grandes ventanales que dejaban entrar mucha luz natural durante el día y hacían que uno no se sintiera como si estuviera en un hospital. "No puedo explicarles la gran diferencia que eso hace", dijo Tipton. Recordó haber visto una tormenta desatarse y sentirse reconfortado al ver todo el movimiento del mundo exterior. “Te recuerda que esta pequeña habitación no es todo lo que hay”.
El interior de esa pequeña habitación puede ser estresante. Los niños necesitaban sondas nasogástricas que van desde la nariz hasta el estómago para complementar lo que podían tomar del biberón, dijo Tipton. Al principio, las enfermeras se encargaban de la alimentación, pero con el tiempo, él empezó a sentirse seguro de que podía hacerse cargo.
“Las enfermeras realmente nos animaron a involucrarnos en el cuidado de nuestros hijos tanto como quisiéramos. Ya fuese para alimentarlos, cambiarlos o bañarlos, no permitieron que nos quedáramos pasmados o que nos hicieran a un lado por nuestra incertidumbre o miedos. Realmente nos animaron a hacernos cargo de la crianza y el cuidado de nuestros hijos.
“El concepto de sala de cuidados conjuntos ofrece una oportunidad para comenzar a practicar cómo será el cuidado en el hogar, incluso en el entorno hospitalario, con el apoyo del personal de enfermería. Así que es casi como tener rueditas de entrenamiento para cuando traes a tu bebé a casa. "Es una oportunidad para que practiques y aprendas y puedas asegurarte de que tanto tú como tu bebé están preparados para el éxito al llegar a casa", dijo.
Afortunadamente, los niños Tipton permanecieron en la UCIN solo nueve días antes de ser dados de alta, pero Jay recordó que otras familias en la unidad habían estado allí mucho más tiempo, convirtiendo sus habitaciones privadas en una extensión de su hogar. Eso era bienvenido, aunque no promovido, dijo, e hizo que la experiencia fuera más cómoda.
Pero lo que más le quedó grabado fue el personal, especialmente el Dr. White.
“Lo que quedó grabado en mi memoria y que nunca olvidaré: Él venía todas las mañanas durante las rondas y estaba en la habitación todo el tiempo que necesitáramos para hablar con nosotros, decirnos cuáles eran nuestros objetivos para el día y responder nuestras preguntas. Y cuando se iba, siempre se daba vuelta y miraba hacia otro lado diciendo: "Es el mejor trabajo del mundo". Y realmente lo decía en serio. Se notaba que no era algo que él simplemente decía”, dijo Tipton. “No se puede cuantificar lo que significa para un paciente tener un médico que no sólo está tan comprometido, sino que además siente tanta alegría por lo que hace”.

Educating Students on Compassionate Care
White is obviously passionate about these fragile NICU babies and their families, but what’s just as clear is his commitment to teaching the next generation of practitioners.
“One of the things that I realized very early on was that they hadn’t prepared me in medical school for much of everything about medicine that wasn’t science—like the social and environmental. And these sorts of things were nothing that we gained training in. And I thought that was really important, not just for people going into neonatology, but doctors in general,” White said.
White now works to fill that gap. As a clinical professor in the Compassionate Care in Medicine minor for future medical professionals in the College of Science, each spring he and Professor Kolberg teach Psychology and Medicine to undergraduates. The course covers topics such as physicians’ well-being, burnout, stress, and compassion. He also guest lectures in Kolberg’s Clinical Embryology course, and focuses on infant and family-centered care.
Educando a los estudiantes sobre la atención compasiva
Obviamente, White siente pasión por estos frágiles bebés de la UCIN y sus familias, pero lo que es igualmente claro es su compromiso de enseñar a la próxima generación de profesionales.
“Una de las cosas de las que me di cuenta muy pronto fue que en la facultad de medicina no me habían preparado para casi todo lo relacionado con la medicina que no fuera ciencia, como las cuestiones sociales y ambientales. Y este tipo de cosas no fueron algo en lo que hayamos recibido formación. Y pensé que eso era realmente importante, no sólo para las personas que se dedican a la neonatología, sino para los médicos en general”, dijo White.
White ahora trabaja para superar esa brecha. Como profesor clínico en la subespecialidad de Atención compasiva en medicina para los futuros profesionales médicos de la Facultad de Ciencias, cada primavera él y la profesora Kolberg enseñan Psicología y Medicina a estudiantes universitarios. El curso cubre temas como el bienestar de los médicos, el agotamiento, el estrés y la compasión. También es profesor invitado en el curso de Embriología Clínica de Kolberg y se centra en la atención centrada en el bebé y la familia.
Back at the hospital, White invites students to volunteer in the NICU and to experience firsthand what parents experience. Conor Sheehan ’24 worked in the NICU for almost three years during his time at Notre Dame.
Sheehan, who worked at the reception desk, recalled: “Multiple times while answering [phone] calls, parents would call to thank one of the nurses or doctors who cared for their child. Many times this was years after their child was discharged. This always stuck with me when thinking about how great the team at the NICU is and how meaningful the work that they do is. From my perspective I saw how hard they worked and how much they cared about their patients through their commitment to their work.”
With hands-on experience, White’s tutelage, and ever-evolving research, the next generation of Notre Dame neonatologists will be well equipped to care for the fragile new lives in NICUs and the families who love them.
De regreso al hospital, White invita a los estudiantes a ser voluntarios en la UCIN y a experimentar de primera mano lo que viven los padres. Conor Sheehan, de 24 años, trabajó en la UCIN durante casi tres años durante su estadía en Notre Dame.
Sheehan, que trabajaba en la recepción, recordó: “Varias veces, mientras respondía llamadas [telefónicas], los padres llamaban para agradecer a una de las enfermeras o médicos que atendieron a su hijo. Muchas veces, esto ocurrió años después de que su hijo fuera dado de alta. Esto siempre quedó conmigo cuando pienso en lo grandioso que es el equipo de la UCIN y lo importante que es el trabajo que realizan. Desde mi perspectiva, vi lo duro que trabajaban y lo mucho que se preocupaban por sus pacientes a través del compromiso con su trabajo”.
Con experiencia práctica, la tutela de White y una investigación en constante evolución, la próxima generación de neonatólogos de Notre Dame estará bien equipada para cuidar las frágiles nuevas vidas en las UCIN y las familias que las aman.
Credits
- Writer: Tara Hunt McMullen
- Photographer: Matt Cashore
Créditos
Escritor: Tara Hunt McMullen
Fotos: Matt Cashore






